Breast Cancer Overview
Introduction
Breast cancer is a disease wherein cells in the breast grow out of control. Like all other cancers, breast cancer is a result of mutations/abnormal changes in genes functional for regulating the growth of cells.
Generally, breast cancer begins either in the lobules or ducts of mammary glands and spreads to the nearby healthy tissues of the breast. However, in rare cases, it could occur in the stromal tissues of the breast.
In >85% of cases, breast cancer is developed due to phenotypic factors involved in the aging process, and genotypic associations are rarely observed for this condition. Many breast cancers do not have obvious symptoms. Few common signs that indicate the possibility of breast cancer are lumps in the breast, change in the shape of the breast, abnormal fluid discharge from nipples, newly-inverted nipple, breast pain, etc. These signs should be self-monitored by women at risk to aid in the early diagnosis by mammography and effective curative treatment.
Breast cancer is the leading cause of cancer in women, and its burden is increasing in developing countries where most of the cases are diagnosed in later stages.1, 2
Classification
The type of breast cancer depends on the cells in the breast that turn into cancerous cells. There exist several types of classification for breast cancer, depending on the stage, histology, TNM grades, function, etc.
Among multiple classifications, breast cancer is generally divided into:
- Histological
- Molecular, and
- Functional classifications.3
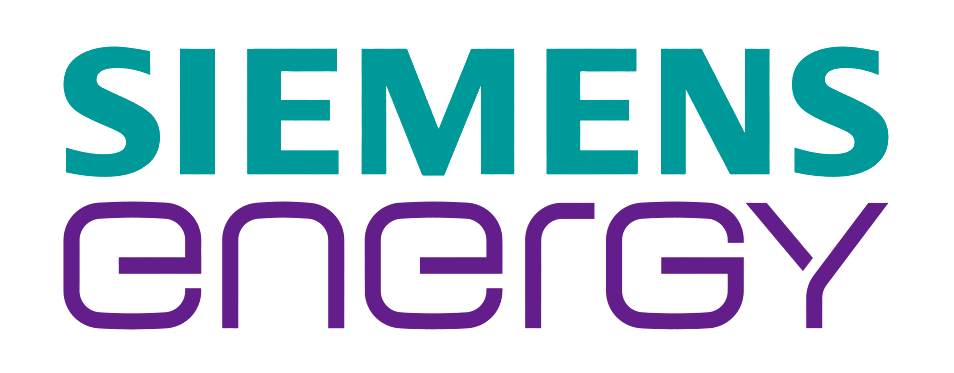
Histological Classification: Most commonly used by clinicians to categorize the heterogeneity found in breast cancer based on architectural features and growth patterns. Breast cancer is broadly classified into in-situ carcinoma and invasive (infiltrating) carcinoma.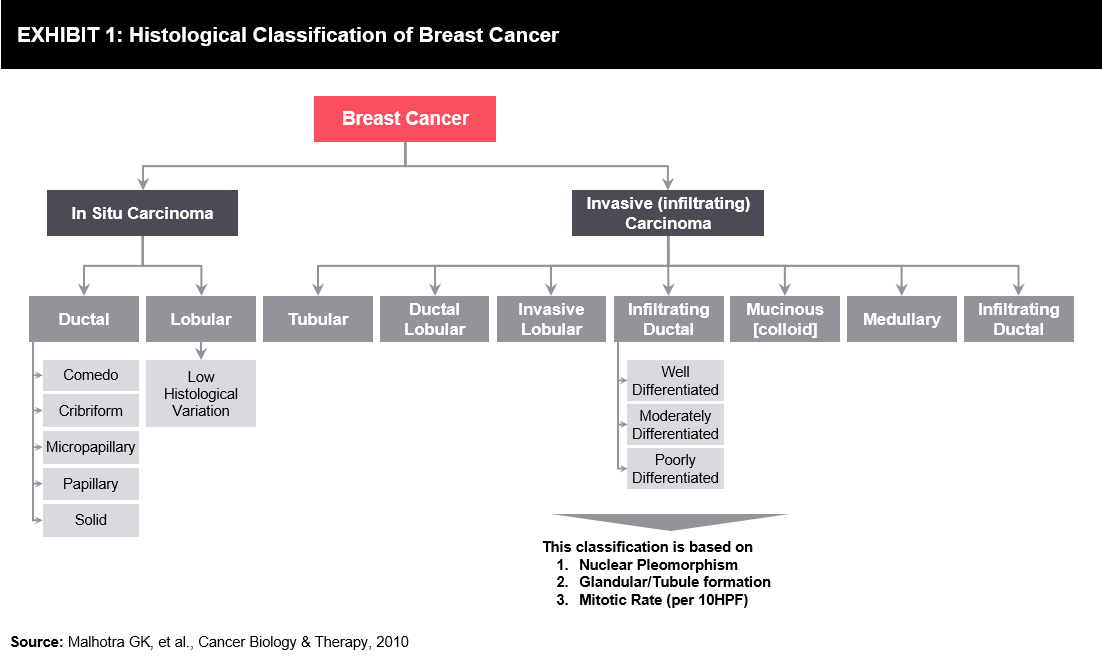
Molecular Classification: This classification is based on the intrinsic molecular subtypes of breast cancer identified by microarray analysis of patient tumor specimens. It provides information on patient-specific prognosis, risk of relapse, and probability for pathological complete response. There are several multi-gene predictors for breast cancer that can be used in the near future.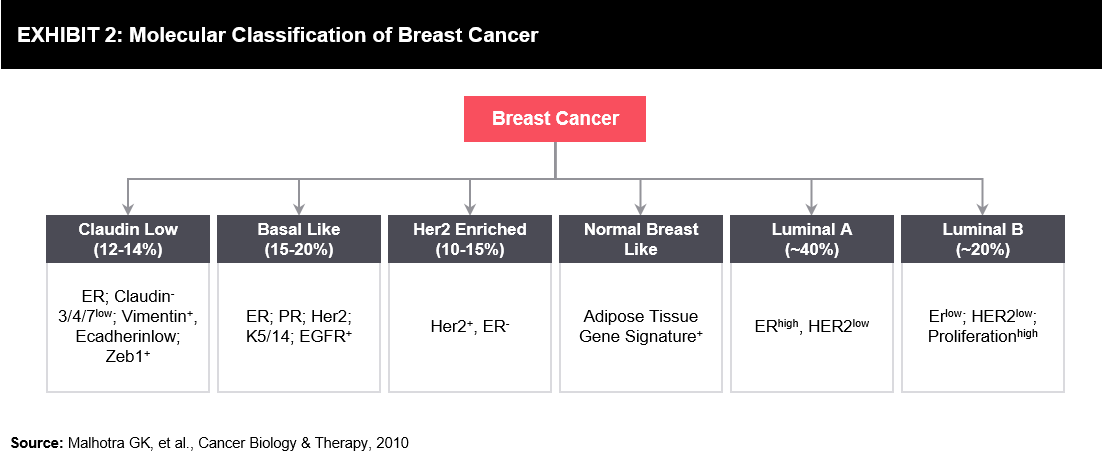
Functional Classification: Functional classification is based on tumor-initiating cells. There are two proposed hypothesis for heterogeneity seen in breast cancer:
- Arises from distinct mammary stem/progenitor cells at various levels within the mammary stem cell hierarchy
- Arises from single mammary stem/progenitor cell being transformed by various oncogenes that give rise to various types of cancer
Epidemiology
Breast cancer is common among women, and it is one of the leading causes of death among them. The incidence rate of breast cancer varies greatly with race and ethnicity. The incidence of breast cancer is higher in developed countries; in contrast, the mortality rate is higher in underdeveloped or developing countries.4
There is a significant increase in the incidence and mortality rates of breast cancer worldwide, which propels the need for early detection, widespread awareness, and effective treatment facilities.
In 2018, there were an estimated 18.1 million new cancer cases and the most common, non-cutaneous breast cancer accounted for 11.6% of total cases, which led to 2.1 million diagnosed cases and subsequently, 0.6 million deaths.5
Incidence
- US6: In the US, ~12% of women develop breast cancer over the lifetime. In 2019, expected diagnosed breast cancer cases will be around 0.27 million. A man’s lifetime risk of breast cancer is about 1 in 883. For women in the US, breast cancer incidence is higher than for any other cancer. Breast cancer is more common in African-American women than in White women under 45 years of age. The risk of developing and dying from breast cancer is lower in Asian, Hispanic, and Native-American women.
- Europe7: In 2018, an estimated number of new breast cancer cases in 28 European Union (EU) countries was 404,920. The incidence increased post the introduction of mammography screening and continues to grow with the aging of the population. A quarter of the breast cancers occurs before the age of 50, and < 5% before age 35. Faulty food habits, obesity, and consumption of alcohol contribute to the rising incidence of breast cancer.
Mortality
- US4: In 2019, around 42,000 women are expected to die due to breast cancer. Mortality rates are higher in African-American women and lower in Asian, Hispanic, and Native-American women.
- Europe5: Breast cancer is the leading cause of death among women in the European region. In 2018, an estimated number of deaths due to breast cancer was around 150,000.
Risk Factors8, 9
- Rise in aging population, especially 50 years of age and older
- Patient undergoing Hormone Replacement Therapy (HRT)
- Long-term combined estrogen-progestogen menopausal therapy
- Women consuming oral contraceptives have a 15-25% higher risk of breast cancer as compared to women who have never used oral contraceptives. Women carry this risk for around 10 years.
- Genetic predisposition, ionizing radiation, low parity, high breast density, and history of atypical hyperplasia are also increasing the risk of breast cancer.
- Few other factors include obesity, alcohol consumption, smoking, western diet, nocturnal working style, diabetes, etc.
Unmet Needs
The prevalence of unmet needs among long-term breast cancer survivors was significantly lower as compared to the unmet needs of patients with survival duration of fewer than 3 years after surgery, and patients with survival duration of less than 1-year post-surgery suffered the greatest unmet needs.10
A study evaluating unmet needs in cancer survivors found that the average number of unmet needs was 2.88. Breast cancer survivors had the highest unmet needs (2.96), and survivors of melanoma/skin cancer had the lowest unmet needs (2.63).11
The unmet needs in breast cancer can be classified into the following: Economic burden, impact on the Quality of Life (QoL), unmet clinical needs, diagnostic challenges, and public awareness.
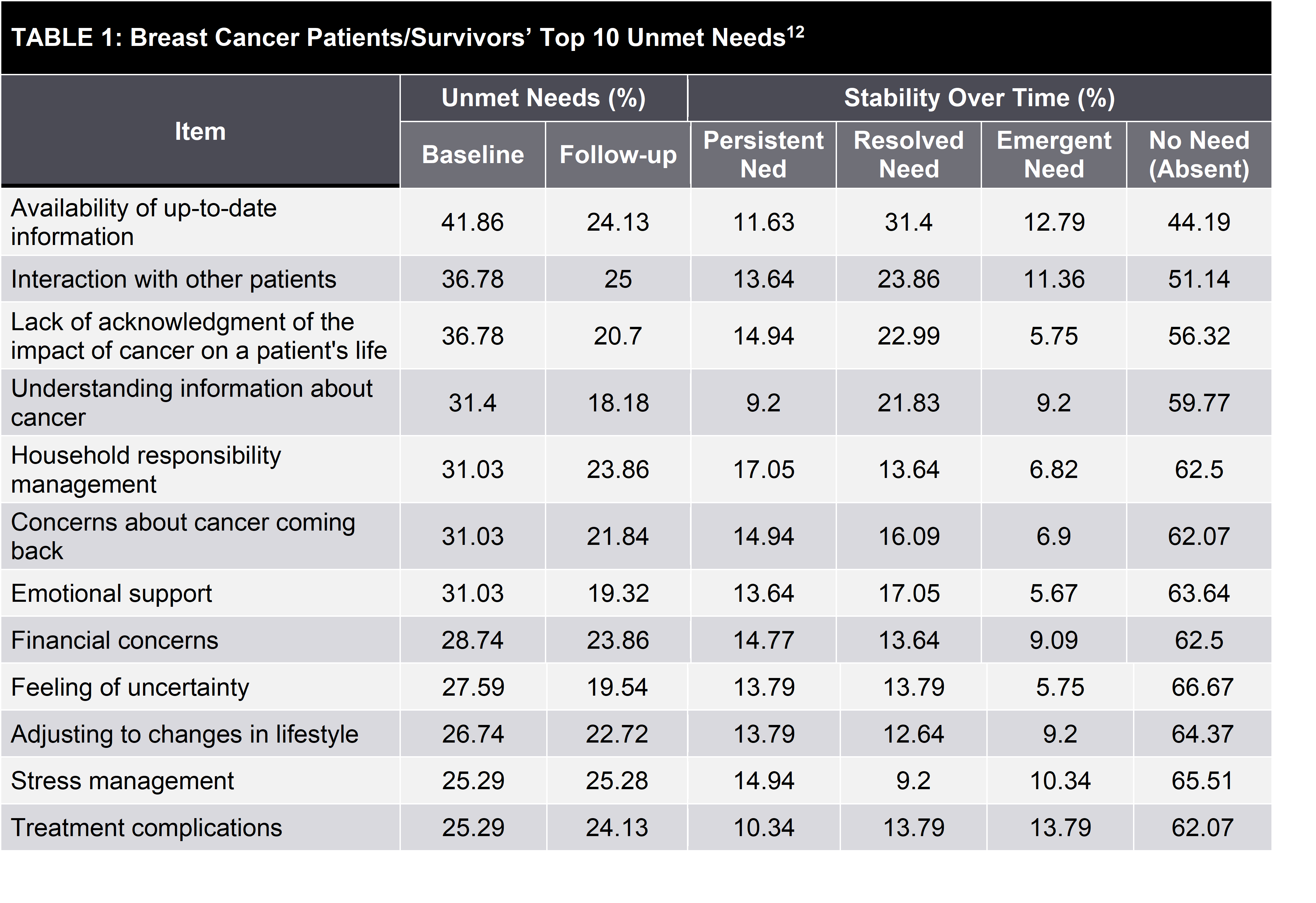
The most common unmet needs among breast cancer patients/survivors based on the data collected in Cancer Survivors’ Unmet Needs (CaSUN) instrument are across physical, healthcare, information, psychosocial, and survivorship domains. Table 1 reports the top 10 unmet needs; most common among them are related to (1) information, (2) interaction with cancer patients/survivors, (3) explaining the impact of cancer to others, (4) stress management, and (5) treatment complications.12
Economic Burden
The cost of treating breast cancer is higher, and it varies widely depending on the geography, stage of the disease, post-treatment complications, and other macro/microeconomic factors.13, 14, 15
- Patients with breast cancer incur ~USD 2000 additional monthly out-of-pocket expenditure vs. case controls without breast cancer in the US (this data could vary in each geography).
- The cost of treating breast cancer increases with the higher stage of cancer at the time of diagnosis.
- Post-treatment complications such as lymphedema or estrogen deficiency symptoms increase the economic burden to a considerable extent.
- There is no clear data available about the complete economic burden of breast cancer owing to multiple factors, such as different methodologies of data capturing, less focus on the long-term indirect impact of breast cancer, etc.
- There is low reimbursement coverage of post-treatment complications, such as lymphedema.
- Though upcoming new treatment options are efficacious and are decreasing mortality rates, they are often costly, primarily affecting the financial life of patients without insurance coverage.
Impact on Quality of Life
Studies show that there are several social and psychological unmet needs in breast cancer. Breast cancer survivors’ face serious challenges based on physical, emotional, and practical (refer Exhibit 5) fronts, as they psychosocially consider themselves as a cancer patient even after complete cure.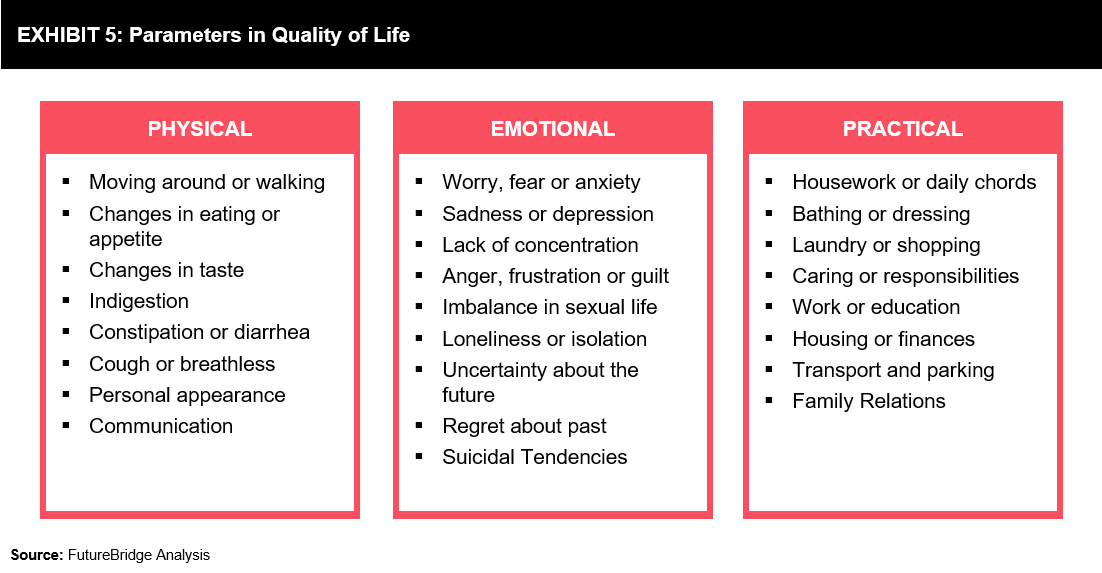
Approximately 40% of breast cancers survivors have mood disorders, which is an important parameter to be monitored rather than focusing only on depression. However, breast cancer survivors are referred to primary healthcare set-ups, where they are not screened entirely for psychosocial distress.16
Under current models of care, especially in developing and underdeveloped countries, many breast cancer patients do not undergo routine follow-ups to assess their physical and emotional state. This is a critical parameter in patient care during the transition from hospital-based to self-management model.17
Emotional distress is very common in breast cancer patients; however, there is limited information available on patient experience and distress screening. An online survey was conducted by the Cancer Support Community during 2013-14 to raise awareness regarding the psychosocial impact of cancer identified top sources (refer Exhibit 6) of distress that were rated as seriously or very seriously concerned.
It was surprising that 43% of respondents were never asked about distress by their healthcare team. 49% respondents reported that fatigue was ‘quite a bit’ or ‘very much’ disruptive in their life and 46% reported intrusive ideation about the financial cost of care. The findings of the survey propel the need for supportive care services and better side-effect management by integrated programs and services across healthcare systems.18
It is important that oncology nurses provide education and emotional support to enhance communication between cancer patients and medical professionals. A survivorship care plan focusing on age-specific issues may be able to improve QOL in young breast cancer survivors.19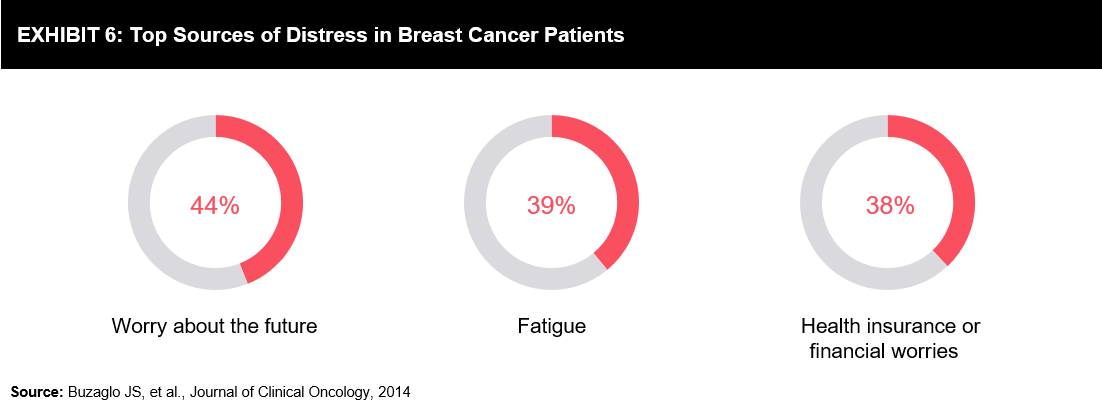
Regular monitoring of QoL using appropriate tools is, therefore, necessary so that cancer care specialists and other health professionals can develop, streamline, and implement specific aspects of cancer care to strategically meet the peculiar needs of patients.20
Clinical Unmet Needs
There are challenges in understanding suitable drug combination or systemic therapy sequence to avoid multidrug resistance and address the intra-tumor heterogeneity.
Standard chemotherapy with the most complete response (22%) is the major treatment option for Triple Negative Breast Cancer (TNBC) subtype. However, patients with TNBC tumors have higher recurrence and metastasis rates than patients with non-TNBC tumors. Due to lack of well-defined molecular targets (ER, PR, and HER2 expression), there are very few therapeutic options available for TNBC. Given the suboptimal treatment outcome with chemotherapy, there is a heightened need for new targeted therapies for TNBC.21
A fixed treatment guideline cannot be defined for advanced breast cancer primarily due to lack of predictive markers of treatment activity. This makes it challenging for treating this patient pool, especially by a less experienced/young oncologist.
A considerable portion of breast cancer survivors face menopausal or estrogen deficiency symptoms, such as insomnia, mood changes, vulvovaginal atrophy, osteopenia, and osteoporosis..22
Diagnostic Challenges
There is a need to improve the monitoring of disease progression by incorporating diagnostics, such as imaging studies and circulating markers into clinical trials.23
The need for biomarkers to assess the response to a systemic therapy has been well-established. However, there is slow progress in identifying reliable biomarkers.
MRI breast cancer screening as an adjunct to mammography has evolved in the field of diagnostics; however, its adaptability in low-income countries or countries with low insurance coverage is challenging due to the cost involved in screening.
There is an immediate need for minimally-invasive, affordable, and highly accurate screening methods, especially in low-income countries, to shift the focus from cost-effectiveness of screening methods to early diagnosis.24
In addition, diagnostic tools to monitor disease recurrence or risks for new primary disease in the long-term are limited.25
The trend towards a more conservative and tailoring treatment using precision medicine is proving beneficial; however, the cost of companion diagnostic identifying genetic mutations for targeted therapies is higher. This could be one of the reasons for lower mortality rates in developed countries though the incidence of the disease is higher.26
Considering the burden of breast cancer, there is a need to shift focus from national guidelines to global guidelines for early diagnosis of breast cancer.
Though early diagnosis services are available in several developed countries, they are mostly limited to the urban population. There is a requirement of increasing the penetration of these services in the rural population for the proactive involvement of women in screening programs.27
Conclusion
The incidence of breast cancer is on the rise, mainly due to the aging population, environmental factors, and lifestyle changes. Mortality of breast cancer is also increasing in underdeveloped regions. There is a need for less costly, structurally designed, and easily accessible screening programs for timely and early diagnosis, mainly in the low income and developing countries. This will reduce the financial burden and mortality rates of breast cancer.
Though there is a tremendous improvement in breast cancer from research, diagnostics, and treatment perspectives, there are few major clinical and diagnostic unmet needs acting as barriers in these advancements. Currently, along with clinical and diagnostic unmet needs, QoL among breast cancer survivors is also being highlighted as a major unmet need. As survival rates are considerably higher in breast cancers when compared with other cancers, the impact of the disease and its treatment on QoL is the highest in breast cancer survivors. The QoL impact includes a significant effect on both physical health and mental health.
Long-term follow-up of breast cancer survivors is necessary to monitor treatment-related clinical complications and QoL. Unfortunately, long-term follow-up of patients/survivors is not achieved in underdeveloped regions, or it is done by a primary physician in most of these regions. Hence, awareness regarding these aspects in general physicians is equally important. Increase in awareness of follow-up examinations serves to be valuable for the research community if, a standardized and effective tool is developed to monitor the QoL and clinical complications in breast cancer survivors.
References
1 CDC
2 Transforming Breast Cancer Together
3 Gautam KM et al., Nov 2010
4 Momenimovahed Z et al., Apr 2019
5 Freddie B et al., Sep 2018
6 Breastcancer.org, Feb 2019
7 Cardoso et al., 2019
8 Europadonna.org, 2018
9 Momenimovahed Z et al., Apr 2019
10 Park BW et al., Jan 2012
11 Burg MA et al., Jan 2015
12 Burris JL et al., Sept 2014
13 Sun L et al., Nov 2018
14 Dean LT et al., May 2019
15 Dean LT et al., March 2019
16 Winter-Martin B., Feb 2019
17 Capelan M et al., Oct 2017
18 Buzaglo JS et al., Sept 2014
19 Miyashita M et al., Nov 2015
20 Okediji PT et al., May 2017
21 Tong CWS et al., June 2018
22 Santen RJ et al., Oct 2017
23 Leo AD et al., Aug 2015
24 Stojadinovic A et al., 2011
25 Partridge AH, March 2019
26 Friese C, Oct 2018
27 Cabanes A et al., Aug 2019
Need a thought partner?
Share your focus area or question to engage with our Analysts through the Business Objectives service.
Submit My Business ObjectiveOur Clients
Our long-standing clients include some of the worlds leading brands and forward-thinking corporations.
- © 2021 Cheers Interactive (India) Private Limited. All rights reserved. FutureBridge ® is a registered trademark of Cheers Interactive (India) Private Limited.